Foundations of economic evaluation
Learning Objectives and Outline
Learning Objectives
Identify theoretical and methodological differences between different economic evaluation techniques.
Understand the concepts of summary measures of health, including quality-adjusted life years (QALYs) and disability-adjusted life years (DALYs).
Be familiar with the steps of valuing costs in economic evaluations.
Outline
Introduction to Economic Evaluations
Types of Economic Evaluations
Who Uses Economic Evaluations
Valuing Health Outcomes
QALYs
DALYs
Valuing Costs
Introduction to Economic Evaluations
Economic Evaluation
Relevant when decision alternatives have different costs and health consequences.
We want to measure the relative value of one strategy in comparison to others.
This can help us make resource allocation decisions in the face of constraints (e.g., budget).
Features of Economic Evaluation
- Systematic quantification of costs and consequences.
- Comparative analysis of alternative courses of action.
Techniques for Economic Evaluation
| Type of study | Measurement/Valuation of costs both alternative | Identification of consequences | Measurement / valuation of consequences |
|---|---|---|---|
| Cost analysis | Monetary units | None | None |
Source: (Drummond et al. 2015)
Cost analysis
Only looks at healthcare costs
Relevant when alternative options are equally effective (provide equal benefits)
- Rarely the case in reality!
Costs are valued in monetary terms (e.g., U.S. dollars)
Decision criterion: often to minimize cost
Techniques for Economic Evaluation
| Type of study | Measurement/Valuation of costs both alternative | Identification of consequences | Measurement / valuation of consequences |
|---|---|---|---|
| Cost analysis | Monetary units | None | None |
| Cost-effectiveness analysis | Monetary units | Single effect of interest, common to both alternatives, but achieved to different degrees. | Natural units (e.g., life-years gained, disability days saved, points of blood pressure reduction, etc.) |
Source: (Drummond et al. 2015)
Cost-Effectiveness Analysis (CEA)
Most useful when decision makers consider multiple options within a budget, and the relevant outcome is common across strategies
- Costs are valued in monetary terms ($)
- Benefits are valued in terms of clinical outcomes (e.g., cases prevented or cured, lives saved, years of life gained, quality-adjusted life years gained)
- Results often reported as a cost-effectiveness ratio
Cost-Effectiveness Analysis
Suppose we are interested in the prolongation of life after an intervention.
Outcome of interest: life-years gained.
The outcome is common to alternative strategies; they differ only in the magnitude of life-years gained.
We can report results in terms of $/Life-years gained
Techniques for Economic Evaluation
| Type of study | Measurement/Valuation of costs both alternative | Identification of consequences | Measurement / valuation of consequences |
|---|---|---|---|
| Cost analysis | Monetary units | None | None |
| Cost-effectiveness analysis | Monetary units | Single effect of interest, common to both alternatives, but achieved to different degrees. | Natural units (e.g., life-years gained, disability days saved, points of blood pressure reduction, etc.) |
| Cost-utility analysis | Monetary units | Single or multiple effects, not necessarily common to both alternatives. | Healthy years (typically measured as quality-adjusted life-years) |
Source: (Drummond et al. 2015)
Cost-Utility Analysis
- Essentially a variant of cost-effectiveness analysis.
- Major feature: use of generic measure of health.
- Quality-Adjusted Life Year (QALY): A metric that reflects both changes in life expectancy and quality of life (pain, function, or both).
- By far the most widely published form of economic evaluation.
We will focus mostly on CEA (especially CUA) throughout the workshop
Techniques for Economic Evaluation
| Type of study | Measurement/Valuation of costs both alternative | Identification of consequences | Measurement / valuation of consequences |
|---|---|---|---|
| Cost analysis | Monetary units | None | None |
| Cost-effectiveness analysis | Monetary units | Single effect of interest, common to both alternatives, but achieved to different degrees. | Natural units (e.g., life-years gained, disability days saved, points of blood pressure reduction, etc.) |
| Cost-utility analysis | Monetary units | Single or multiple effects, not necessarily common to both alternatives. | Healthy years (typically measured as quality-adjusted life-years) |
| Cost-benefit analysis | Monetary units | Single or multiple effects, not necessarily common to both alternatives | Monetary units |
Cost-Benefit Analysis
- Also known as Benefit-Cost Analysis
- Relevant for resource allocation between health care and other areas (e.g., education)
- Costs and health consequences are valued in monetary terms (e.g., U.S. dollars)
- Valuation of health consequences in monetary terms ($) is obtained by estimating individuals willingness to pay for life saving or health improving interventions.
- e.g.: US estimate of value per statistical life ~$9 million
- Cost-benefit criterion: the benefits of a program > its costs
- Notice that we’re not making comparisons across strategies–only comparisons of costs and benefits for the same strategy
- To read more: Robinson et al, 2019
Cost-Benefit Analysis
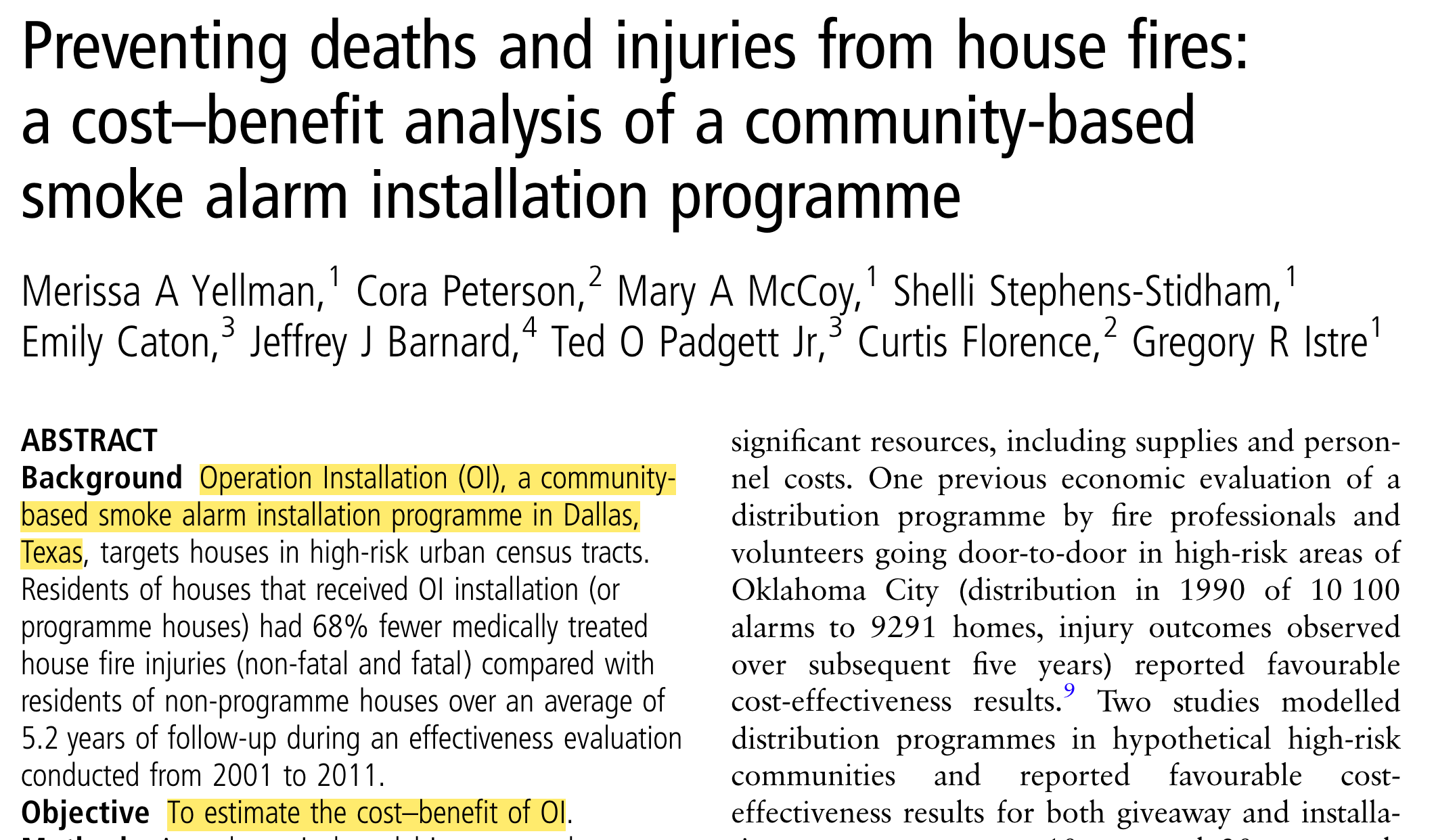
https://pubmed.ncbi.nlm.nih.gov/28183740/
Cost-Benefit Analysis
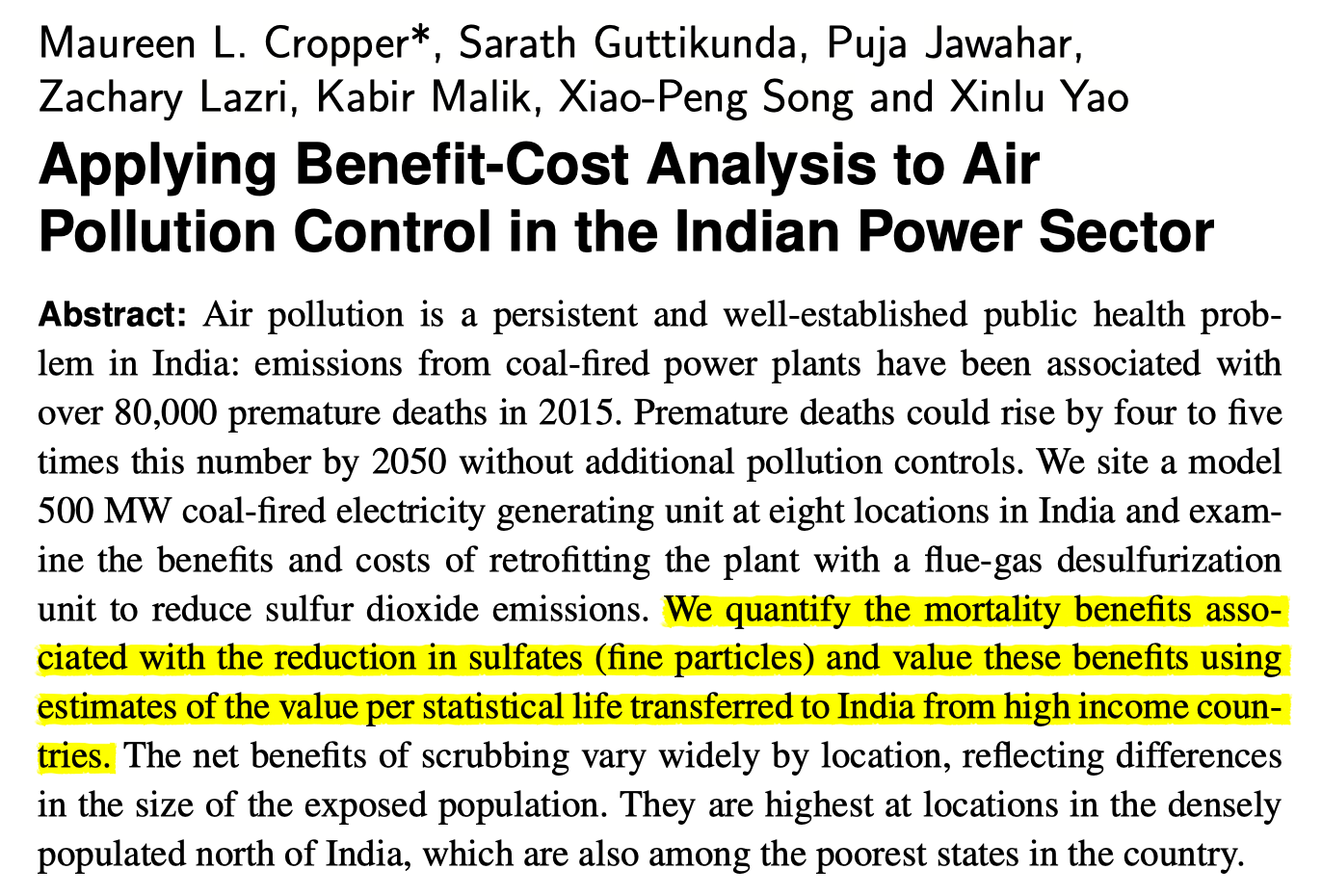
https://www.cambridge.org/core/product/identifier/S2194588818000271/type/journal_article
Who uses economic evaluations?
Health Technology Advisory Committees
PBAC (Pharmaceutical Benefits Advisory Committee in Australia)
Canada’s Drug and Health Technology Agency
NICE (The National Institute for Health and Care Excellence, UK)
Brazil’s health technology assessment institute
Groups developing clinical guidelines
WHO
CDC
Disease-specific organizations: American Cancer Society; American Heart Association; European Stroke Organisation
Regulatory agencies:
FDA (U.S. Food and Drug Administration)
EPA (U.S. Environmental Protection Agency)
CEAs: Identifying Alternatives
Identifying Alternatives
Decision modeling / economic evaluation requires identifying strategies or alternative courses of action.
These alternatives could include different therapies / policies / technologies.
Or, our alternatives could capture different combinations or sequences of treatment (e.g., what dose? what age to start?)
Once we have identified the alternatives, we’ll want to quantify their associated consequences in terms of:
Health outcomes
Costs
CEA components
\[ \frac{\text{(Cost Intervention A - Cost Intervention B)}}{\text{(Benefit A - Benefit B)}}\]
Valuing Health Outcomes
Why summary measures of health?
QALYs and DALYs both provide a summary measure of health
Allow comparison of health attainment / disease burden
Across diseases
Across populations
Over time etc.
QALYs
Origin story: welfare economics
- Utility = holistic measure of satisfaction or wellbeing
With QALYs, two dimensions of interest:
length of life (measured in life-years)
quality of life (measured by utility weight, usually between 0 and 1)
QALYs
QALY: A metric that reflects both changes in life expectancy and quality of life (pain, function, or both)
1 = perfect health; 0= death; Sum of weight*duration of life = quality-adjusted life expectancy
Example: Patient with coronary heart disease (with surgery)
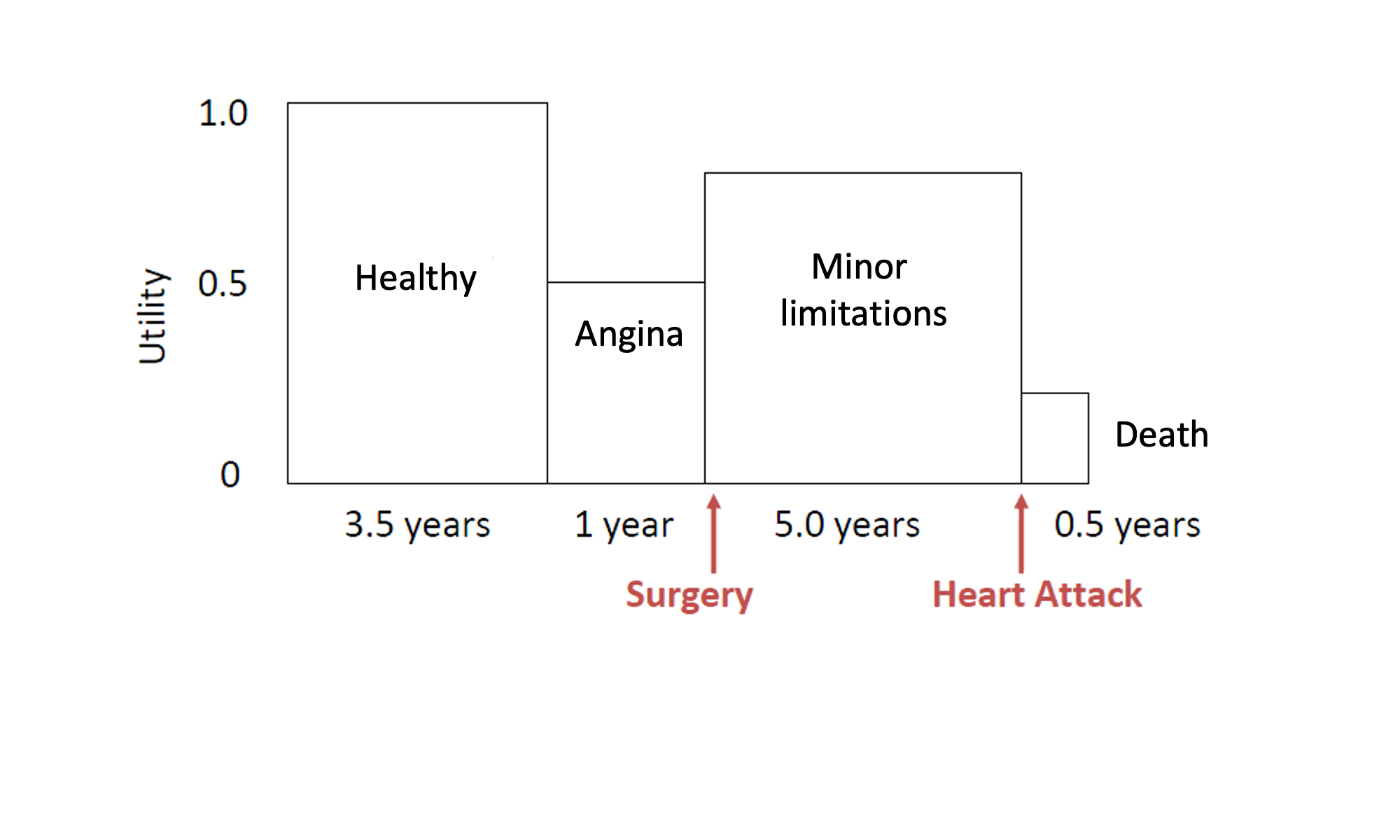
Example: Patient with coronary heart disease (with surgery)
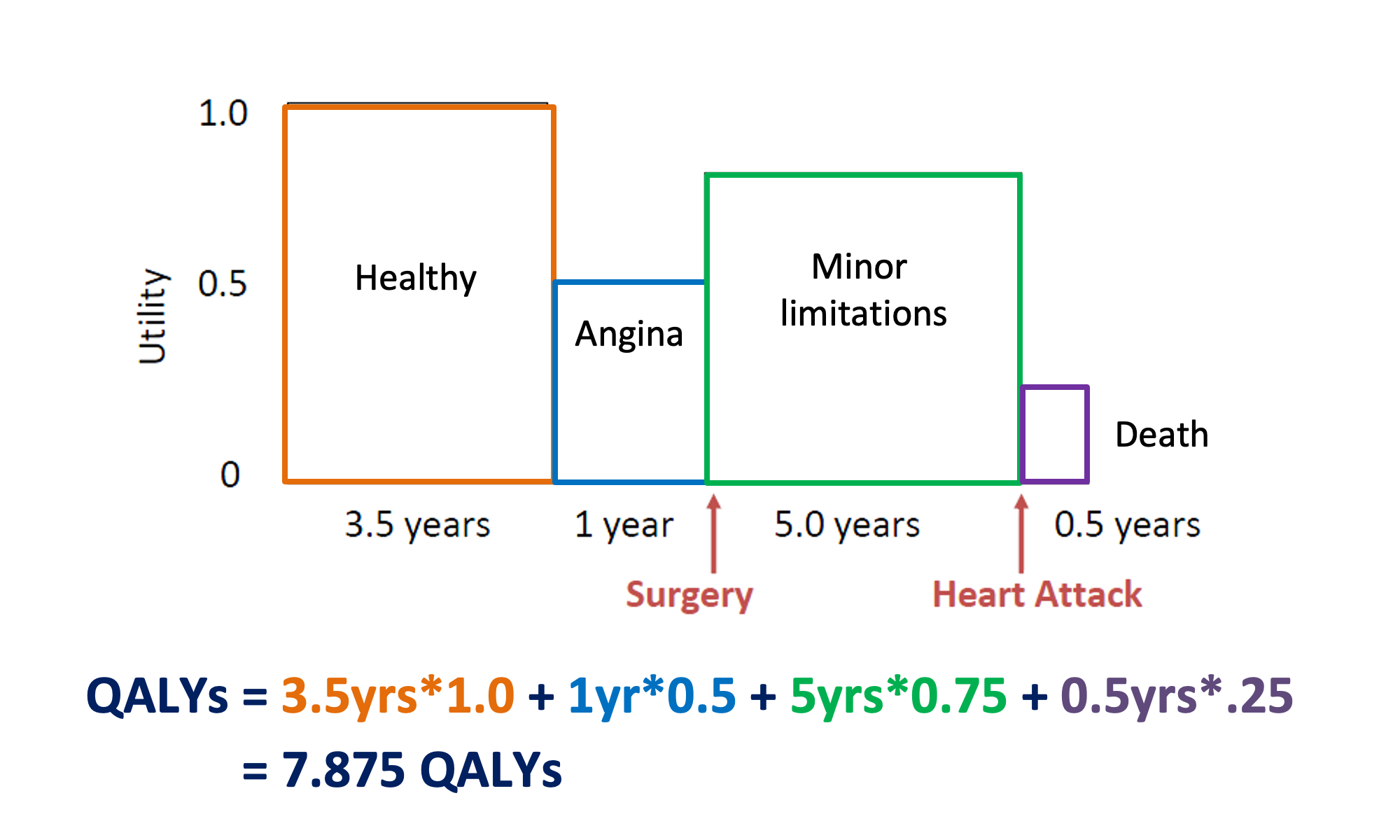
Example: Patient with coronary heart disease (without surgery)

Example: Patient with coronary heart disease
- With surgery: 7.875 QALYs
- Without surgery: 6.625 QALYs
- Benefit from surgery intervention:
In QALYs: 7.875 – 6.625 QALYs = 1.25 QALYs
In life years: 10 years – 10 years = 0 LYs
Utility weights – How are they obtained?
Utility weights for most health states are between 0 (death) and 1 (perfect health)
Direct methods
Standard gamble
Time trade-Off
Rating scales
Indirect methods:
EQ-5D
Other utility instrument: SF-36; Health Utilities Index (HUI)
Direct methods - Standard Gamble (SG)
“What risk of death you would accept in order to avoid [living with stroke the rest of your life] and live the rest of your life in perfect health?”
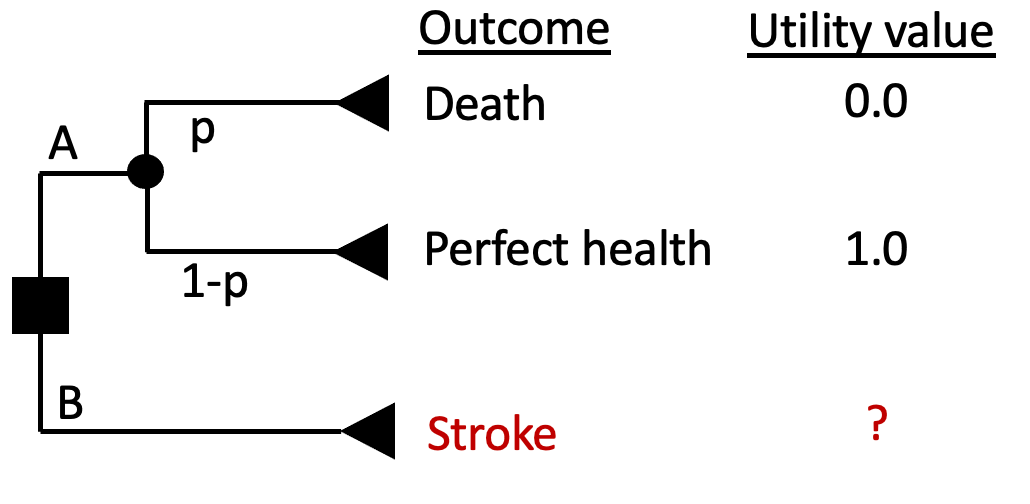
How bad is having a stroke?
As a result of a stroke, you
Have impaired use of your left arm and leg
Need some help bathing and dressing
Need a cane or other device to walk
Experience mild pain a few days per week
Are able to work, with some modifications
Need assistance with shopping, household chores, errands
Feel anxious and depressed sometimes
Direct methods - Standard Gamble (SG)
“What risk of death you would accept in order to avoid [living with stroke the rest of your life] and live the rest of your life in perfect health?”
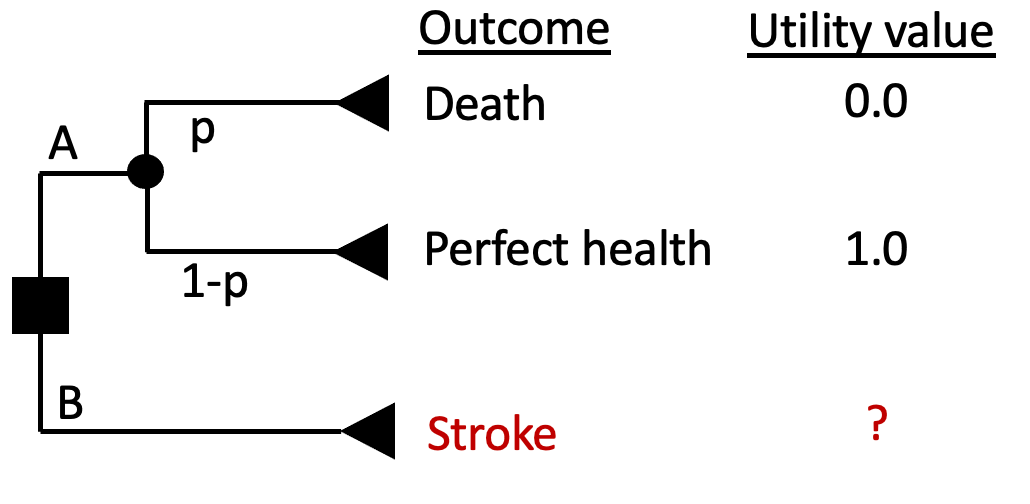
- Find the threshold \(p_T\) that sets EV(A) = EV(B)
- Assume respondent answered that they would be indifferent between A and B at a threshold \(p_T = 0.2\)
- Then U(Stroke) = \(p_T\)*U(Death) + \((1-p_T)\)*U(Perfect Health) = 0.2*0 + (1-0.2)*1 = 0.8
Direct Methods - Time Trade-Off (TTO)
An alternative to standard gamble
Instead of risk of death, TTO uses time alive to value health states
Does not involve uncertainty in choices
Task might be easier for some respondents compared to standard gamble
Direct Methods - Time Trade-Off (TTO)
“What portion of your current life expectancy of 40 years would you give up to improve your current health state (stroke) to ‘perfect health’?”
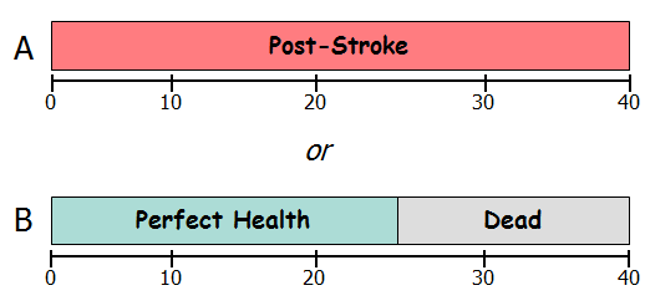
U(Post-Stroke) * 40 years = U(Perfect Health) * 25 years + U(Dead) * 15 years
U(Post-Stroke) * 40 years = 1 * 25 years + 0 * 15 years
U(Post-Stroke) = 25/40 = 0.625
SG vs TTO
SG represents decision-making under uncertainty; TTO is decision-making under certainty
TTO might inadvertently capture time preference (i.e., we might value health in the future less than we do today) as opposed to only valuing the health states
Risk posture is captured in SG (risk aversion for death) but not in TTO
Utility values from SG usually > TTO for same state
Direct methods – Rating scales
“On a scale where 0 represents death and 100 represents perfect health, what number would you say best describes your health state over the past 2 weeks?”
- Problem: It does not have the interval property we desire
- A value of “90” on this scale is not necessarily twice as good as a value of “45”
Visual Analogue Scale (VAS)
The Visual Analog Scale (VAS) is a commonly-used rating scale
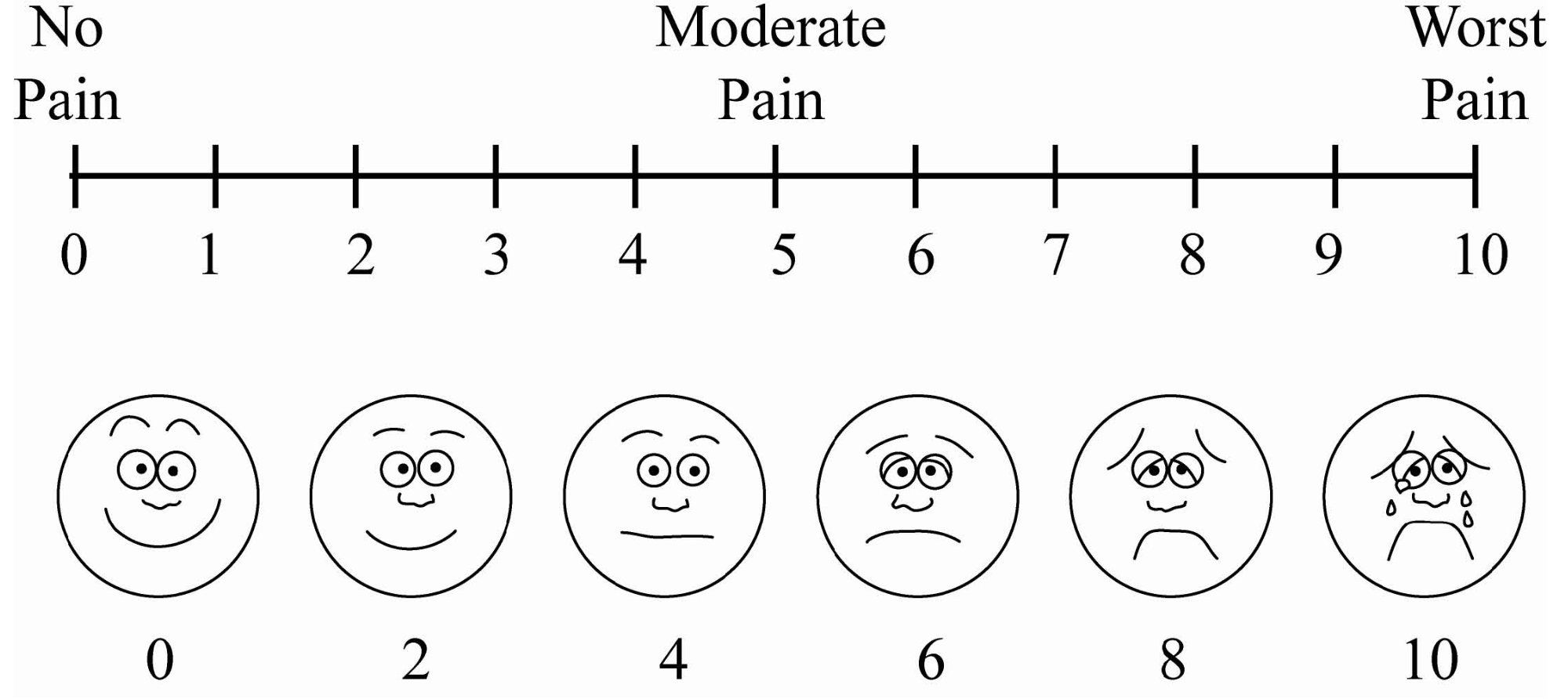
Direct methods – Rating scales
- Easy to use: Rating scales often used where time or cognitive ability/literacy prevents use of other methods
- Very subjective and prone to more extreme answers! Usually, utilities for VAS < TTO < SG
Practical issue – keep an eye out for “cheaters”
Hypothetical “cheating” example:
Drug company X has discovered a drug that prevents diabetes but causes migraines (side-effect)
They use VAS to estimate the utility of diabetes in their decision model and SG to estimate the utility of migraines
Is there a problem here? (yes, there is!!)
Recall, usually utilities for VAS < TTO < SG
Thus, this approach overstates the benefit by using a lower U(Diabetes) and higher U(migraines)
Indirect Methods - EQ-5D
System for describing health states
5 domains: mobility; self-care; usual activities; pain/discomfort; and anxiety/depression
3 levels: 243 distinct health states (e.g. 11223)
Valuations elicited through population based surveys with VAS, TTO
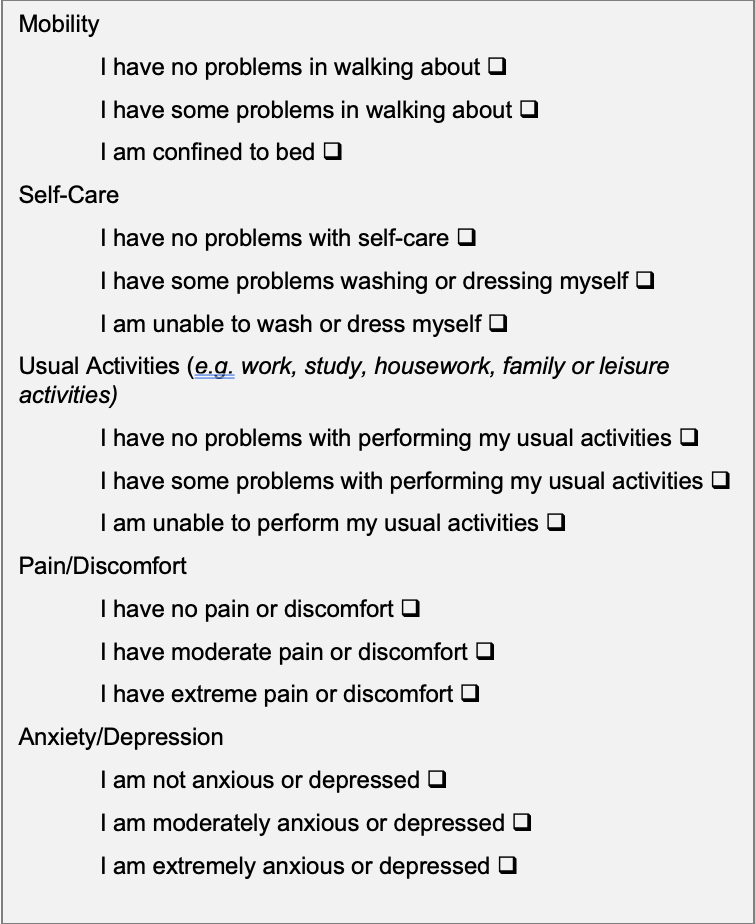
System for describing health states
5 domains: mobility; self-care; usual activities; pain/discomfort; and anxiety/depression
3 levels: 243 distinct health states (e.g. 11223)
Valuations elicited through population based surveys with VAS, TTO
Off-the-shelf numbers for your own CEAs?
- Large scale utility studies
- Balancing tradeoffs between different measures
- Sensitivity analyses!
- Tufts CEA registry
- Alongside RCTs
DALYs
QALY: “0” = death; “1” = perfect health
DALY: “0” = perfect health; “1” = death
- QALY measures the number of healthy years gained (uses preference-based utility weights)
- DALY measures the number of healthy years lost (uses standardized disability weights)
Source: ghcearegistry.org
DALYs
A measure of population ill-health based on “years of life lost” due to premature mortality (Anand & Reddy LSE 2019).
Origin story: Global Burden of Disease Study
Deliberately a measure of health, not welfare/utility
Similar to QALYs, two dimensions of interest:
length of life (differences in life expectancy)
quality of life (measured by disability weight)
DALYs
DALYs = YLL + YLD
- YLL (Years of Life Lost): The # of life years a person could have expected to live had they not died
- YLD (Years Lived with Disability)
DALYs = YLL + YLD
Years of Life Lost (YLL): changes in life expectancy; time lost due to premature mortality
Different approaches to identifying the time lost due to premature mortality:
Age specific risks of mortality; maximum length of life observed in modern world: “synthetic life table”; irrespective of country; socioeconomic characterstics/etc. where death occurs
Dependent on a person’s country of residence & other factors in which the death occurs
Approach depends on purpose of study
- Synthetic life table: Quantify disease burden across countries in relation to normative benchmark and/or in light of global justice and resource re-allocation to low-income countries
- Country-specific life table: Assessing alternative disease interventions in Uganda; how many expected years of life are lost due to a disease in conditions specific to Uganda.
DALYs = YLL + YLD
Example: Calculated from synthetic life table
YLL example: Providing HIV treatment delays death from age 30 to age 50
Life years gained = 20 years
YLL?
Synthetic, Reference Life Table
| Age | Life Expectancy | Age | Life Expectancy |
|---|---|---|---|
| 0 | 88.9 | 50 | 39.6 |
| 1 | 88.0 | 55 | 34.9 |
| 5 | 84.0 | 60 | 30.3 |
| 10 | 79.0 | 65 | 25.7 |
| 15 | 74.1 | 70 | 21.3 |
| 20 | 69.1 | 75 | 17.1 |
| 25 | 64.1 | 80 | 13.2 |
| 30 | 59.2 | 85 | 10.0 |
| 35 | 54.3 | 90 | 7.6 |
| 40 | 49.3 | 95 | 5.9 |
| 45 | 44.4 |
Source: http://ghdx.healthdata.org/record/ihme-data/global-burden-disease-study-2019-gbd-2019-reference-life-table
Synthetic, Reference Life Table
| Age | Life Expectancy | Age | Life Expectancy |
|---|---|---|---|
| 0 | 88.9 | 50 | 39.6 |
| 1 | 88.0 | 55 | 34.9 |
| 5 | 84.0 | 60 | 30.3 |
| 10 | 79.0 | 65 | 25.7 |
| 15 | 74.1 | 70 | 21.3 |
| 20 | 69.1 | 75 | 17.1 |
| 25 | 64.1 | 80 | 13.2 |
| 30 | 59.2 | 85 | 10.0 |
| 35 | 54.3 | 90 | 7.6 |
| 40 | 49.3 | 95 | 5.9 |
| 45 | 44.4 |
Source: http://ghdx.healthdata.org/record/ihme-data/global-burden-disease-study-2019-gbd-2019-reference-life-table
DALYs = YLL + YLD
Years of Life Lost (YLL): changes in life expectancy, calculated from comparison to synthetic life table
YLL example: Providing HIV treatment delays death from age 30 to age 50
Life years (LYs) gained: 20 years
YLL: LE(50) - LE(30) = 39.6 - 59.2 = -19.6 DALYs = 19.6 DALYs averted
Note
YLL (measured as DALYs averted) \(\neq\) LYs gained!
DALYs = YLL + YLD
Years Lived with Disability (YLD): calculated similar to QALYs, utility weight ≈ 1 - disability weight
YLD example: Effective asthma control for 10 years
Disability weight (uncontrolled asthma) = ?
Disability weight (controlled asthma) = ?
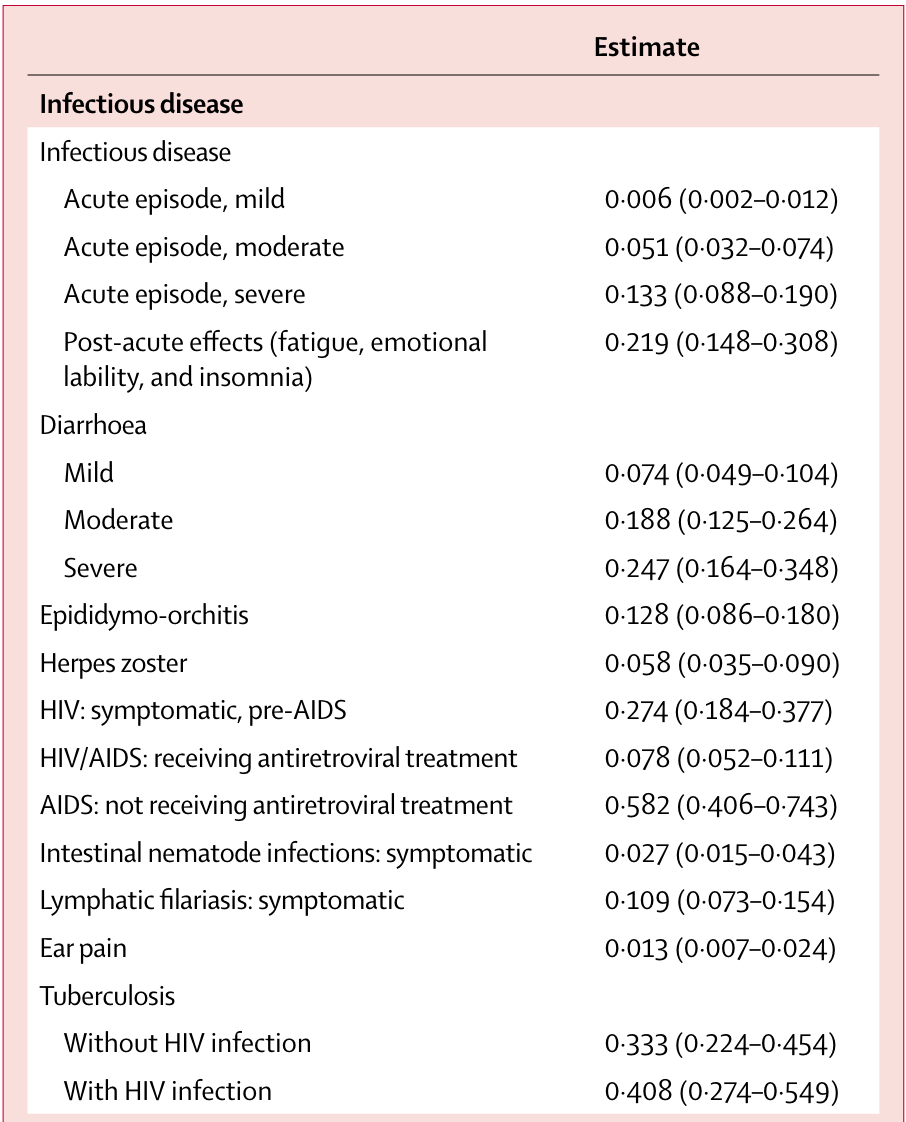
Disability Weights
- Common values for small set of named health conditions (e.g. early/late HIV, HIV/ART)
- First iteration: expert opinion
- Second iteration: Pop-based HH surveys in several world regions (13,902 respondents)
Paired comparison of two health state descriptions which worse
Probit regression to calculate disability weights
235 unique health states
DALYs = YLL + YLD
Years Lived with Disability (YLD): calculated similar to QALYs, utility weight ≈ 1 - disability weight
YLD example: Effective asthma control for 10 years
Disability weight (uncontrolled asthma) = 0.133
Disability weight (controlled asthma) = 0.015
YLD = 10 * 0.015 - 10 * 0.133 = -1.18 DALYs = 1.18 DALYs averted
DALYs for CEA
- Recommended calculation approach has changed over time (age weighting, discounting, now both out)
- Some will calculate a “QALY-like” DALY, using utility weight = 1- disability weight
- Discounting still generally done for CEA (will be covered in Lecture 7!)
Important
Common practice
- High-income setting: QALYs
- Low- and middle- income setting = DALYs***Since disability weights are freely & publicly available (these weights are required for DALY calculations), it can reduce costs/time/resources compared to collecting QALY estimates
Valuing Costs
Steps
Identify
Measure
Value
We can identify different types of healthcare costs
Direct Health Care Costs
Hospital, office, home, facilities
Medications, procedures, tests, professional fees
Direct Non-Health Care Costs
- Childcare, transportation costs
Time Costs
- Patient time receiving care, opportunity cost of time
Productivity costs (‘indirect costs’)
impaired ability to work due to morbidity?
lost economic productivity due to death?
friction costs
We can measure costs using different approaches
Micro-costing (bottom-up)
- Measure all resources used by individual patients, then assign the unit cost for each type of resource consumed to calculate the total cost
Gross-costing (top-down)
- Estimate cost for a given volume of patients by dividing the total cost by the volume of service use
Ingredients-based approach (P x Q x C)
Probability of occurrence (P)
Quantity (Q)
Unit costs (C)
Adjustments needed for Valuing Costs
Discounting
Adjusting for currency and currency year
Will cover these adjustments in Lecture 7!
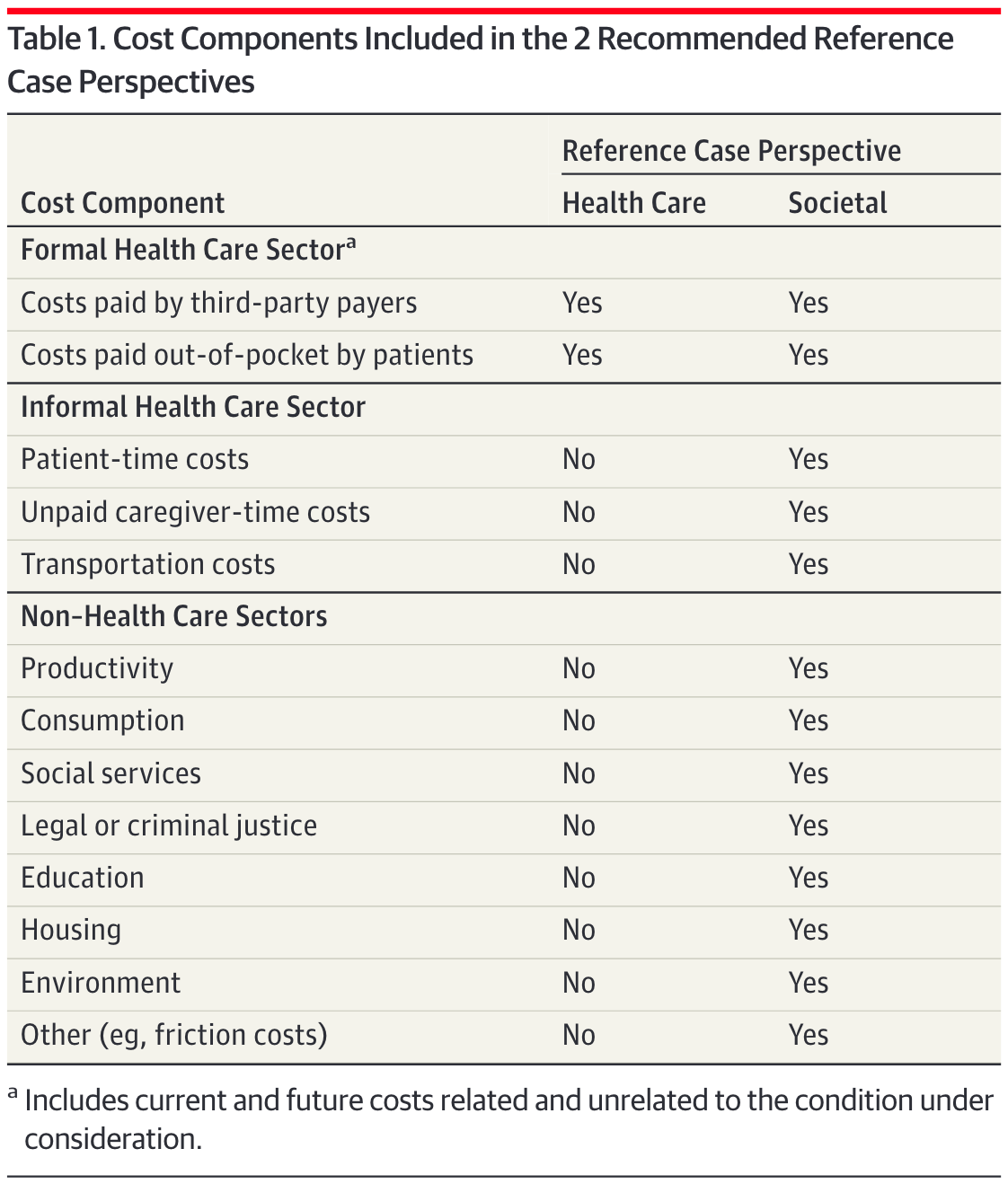
Whose perspective?
Sanders GD, Neumann PJ, Basu A, et al. Recommendations for Conduct, Methodological Practices, and Reporting of Cost-effectiveness Analyses: Second Panel on Cost-Effectiveness in Health and Medicine. JAMA. 2016;316:1093–1103.